The medical coding industry is one that people often misunderstand. It can be frustrating trying to learn and understand not only the various sets of codes, but also the industry as a whole. However, medical cording is essential for medical billing and if you are looking to get reimbursed by insurance companies, your facility will need to bite the bullet and embrace medical cording.
Why Do You Need to Use Medical Coding?
While it might seem like you can simply list out symptoms, procedures and diagnoses and send them out to insurance companies, there is way too much information being sent back and forth and mistakes can be greatly increased if there is no strict code to follow. Some cases are very straightforward and that method may work, but when you get to more complicated doctor visits with multiple symptoms, tests, diagnoses and procedures, there can be a lot of confusion created. As injuries and illnesses get more complicated – and therefore more costly – the insurance company will want more information, which means that your staff will be spending a lot of time listing everything out for them. With over a billion patient visits every year, can you imagine how overloaded insurance providers will be? You will find yourself waiting longer for reimbursements, and the likelihood that there is an issue with the paperwork grows exponentially.
Coding Creates Uniformity
There are thousands and thousands of medical facilities throughout the country. Can you imagine the confusion that is created by different facilities differing procedures and explanations? By utilizing a set coding system, every facility uses the same language, so to speak. That means that insurance companies can handle requests faster, data can be tracked more efficiently, and the health care system as a whole benefits.
Different Types of Coding
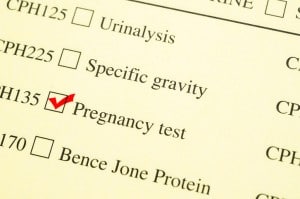
You understand the important of coding, but do you know the different sets of code that are utilized? ICD codes are diagnostic codes that are used to describe the reasons behind injuries, illnesses and death. CPT codes are used to document the procedures that are performed in medical facilities, and HCPCS codes correspond to the procedures, services and equipment that isn’t already covered by CPT codes. These sets of codes are crucial for ensuring that your documents are being coded properly, so that you are reimbursed accordingly.
Do You Need Our Help With Medical Coding?
Medical coding can be an overwhelming process that your staff struggles to work through. At HCC Coders, we strive to offer medical coding services to enhance the bottom line of your business, while simultaneously allowing you to provide the best medical care to your patients. We know how frustrating it can be to try and keep up with your coding tasks, which is why we offer our quality coders to assist with your projects.